Market Town : Tilney1 : Watching a plane fall from the sky, aflame.

“You get depressed about your diagnosis and what people think about you. I always think about it, it is a severe mental illness, that I have and if you’re thinking about these things, in the loneliness that I have and you hear all the sounds, see the shapes… it’s very difficult for me.”
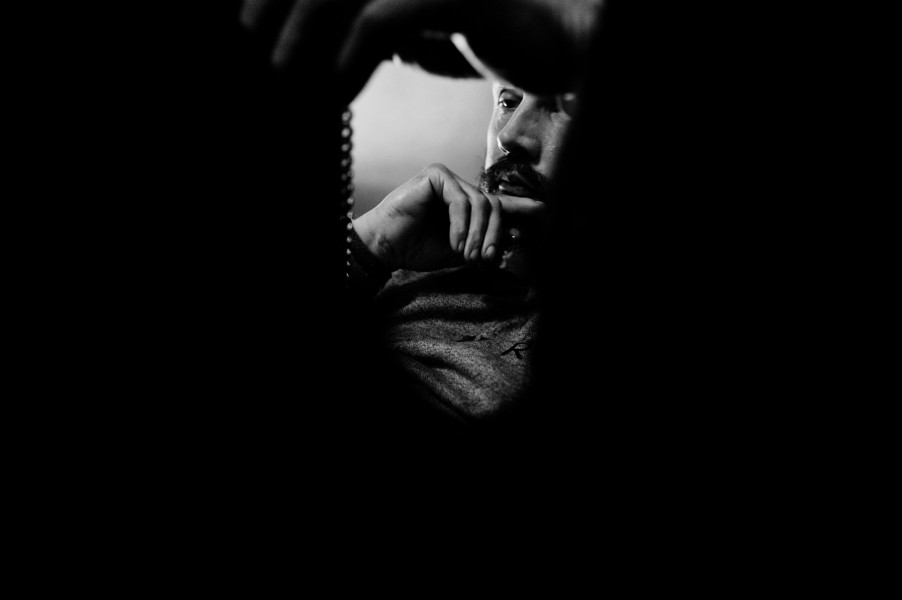
It was as though watching a man drowning beneath the ice. I see him hitching for breath, chest heaving, eyes wild, fingers whipping at the indifferent, almost invisible, wall above.
I can do nothing but witness.
I, as trapped in these moments, as he imprisoned below, our eyes now connected. His fear, his absolute and consuming terror is loud within his gaze, as loud, I imagine, as his frozen water screams, muted by the barrier between us.
His fear resonates, pulsates with the realisation that we are both completely aware of what is happening and both completely helpless to alter a single fucking thing.
It was watching time run out.
It was watching a trapped man caught in the throes of desperation.
It was watching a car crash in slow motion.
It was watching a plane fall from the sky, aflame.
It was face pressed to the observation slit upon the cell of a forgotten and falsely imprisoned man in solitary confinement.
It was each and all of these things.
It was as though they were all real.
It was and is, this real.
Witnessing Tilney1’s battle with Paranoid Schizophrenia over the course of the past 12 months, his medication changes, his endurance in isolation, his fight to exist and to navigate existence with and often without the regular support and contact with professional care teams, has been both terrifying and illuminating.
Living alone can often be a vicious limbo. Coupled with Tilney1’s symptoms, fears and the crippling effects of his diagnosis and medications, life for Tilney1 has been brutal.
A change in C.P.N’s (Community Psychiatric Nurse) home visits from crisis teams dwindling, due to their own battle with staffing and budget cuts to local mental health services, led to Tilney1 missing medication. It began, slowly. A missed pill here, a skipped pill there. Soon, bags of unopened medication were stockpiled within his bathroom.
With each pill missed, a little more of Tilney1’s character traits, for years suppressed by medication, would rush to the surface. It was a dangerous game, addictive. With each pill missed, a little more self-confidence and a little more, a little more, a little more.
A dangerous game, for soon, without correct and timetabled medication, with no medicinal brakes nor physical checks to slow his diagnosis and it’s multiple symptoms, this initial rush of confidence, of euphoria, would lead to mania and manic episodes.
A potent and cruel trick, being so close to a remembered self, to be led by a hand, so soothing, to seem in reality to be escaping the trap of the prison within the self, yet all the while being led to the inevitable crash. Especially cruel as Tilney1 was able to watch all this happening to himself, to have that insight, possess that awareness, yet to be completely incapable of intervening, of stopping, to be trapped beneath the ice, screaming for a way out.

Lost in a memory loop.

Tilney1’s paintings, collage work and writings, made in almost constant isolation, fill his apartment.

Apartment.

Though the news is often a source of great stress, Tilney1 pays particular attention to the Labour leadership election.
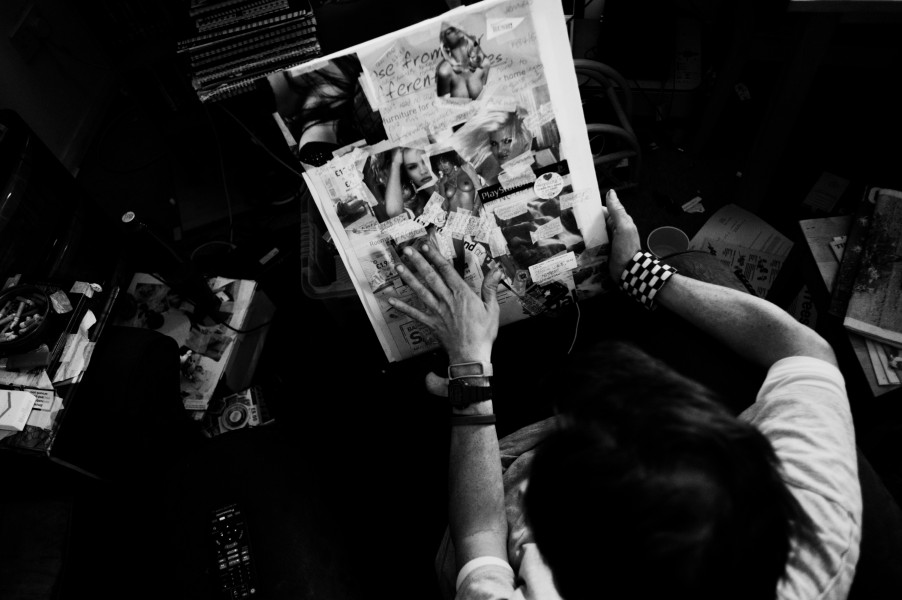
Working on a mixed media collage.

Days and nights are spent reading, trying to combat a mind increasingly unquiet.
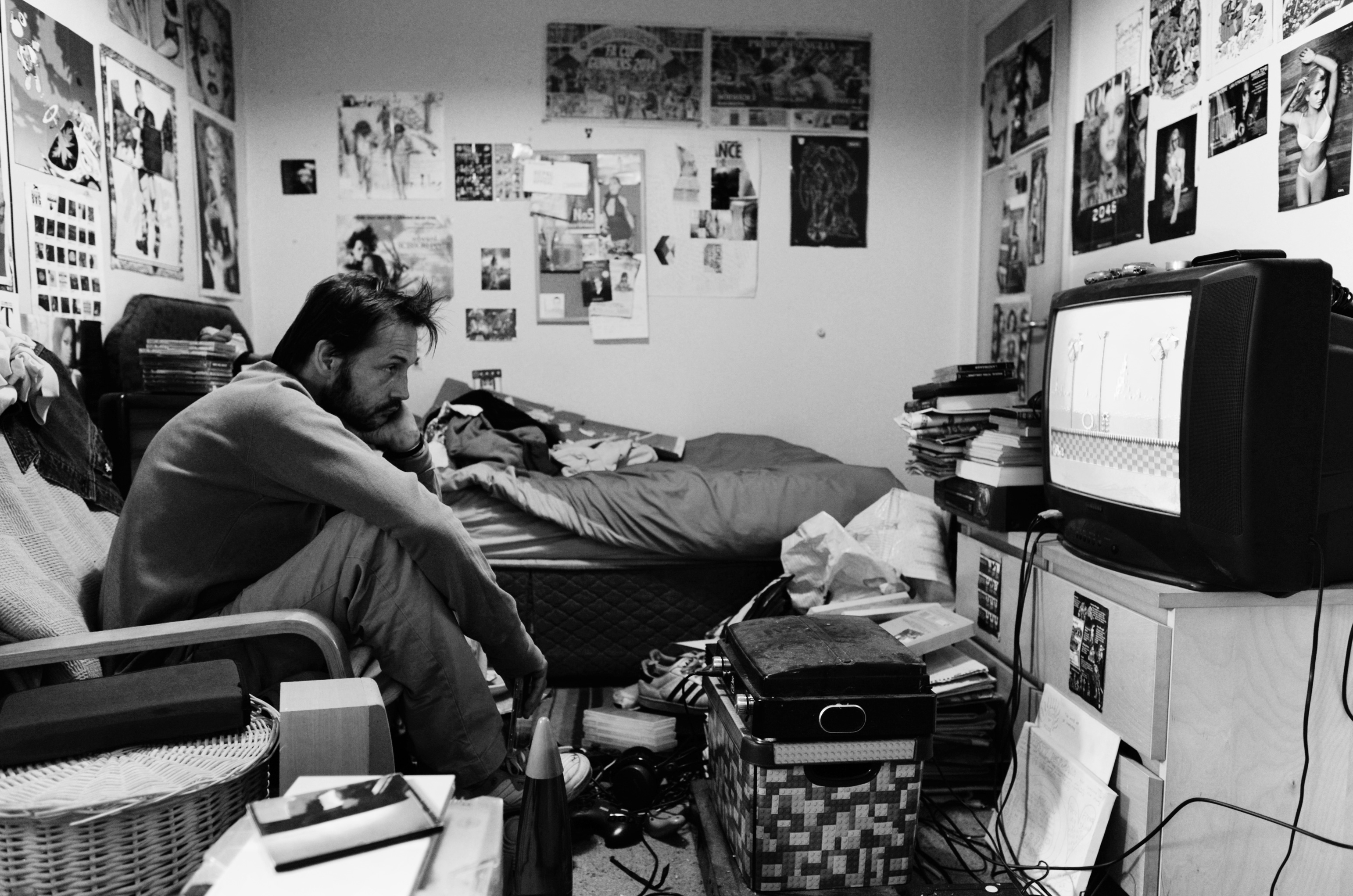
Killing time.

Reading.
Apartment.

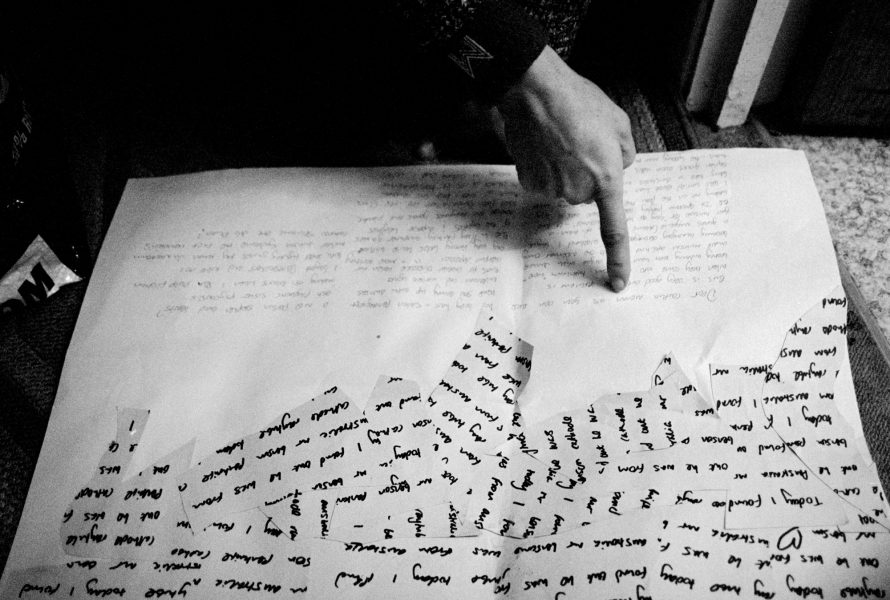
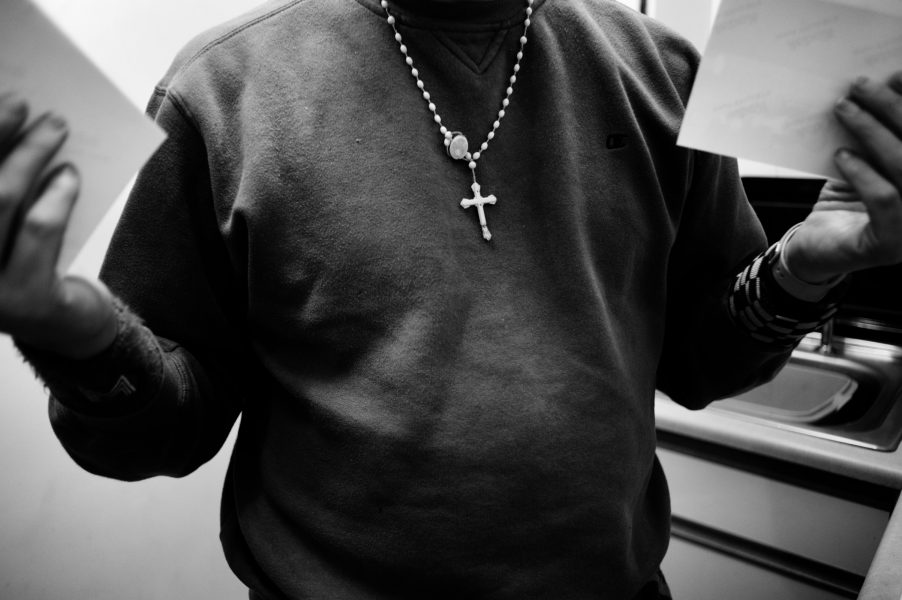
Tilney1 explaining the pain of isolation, days without seeing a living soul and how in the absence of company, the links, delusions and obsessive behaviour gains a damaging momentum.

Working on a journal filled with collage and writings.

Painted nails.
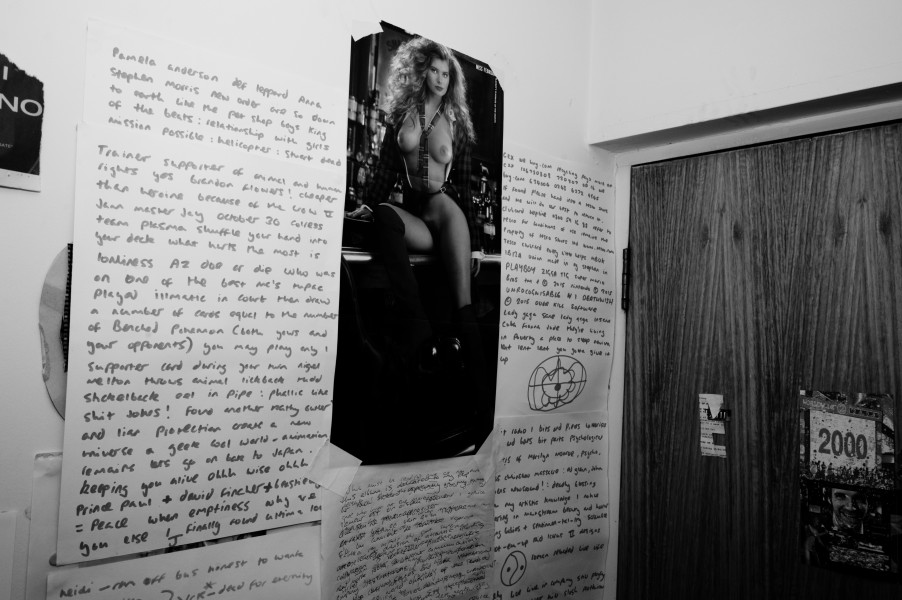
Wall collages.
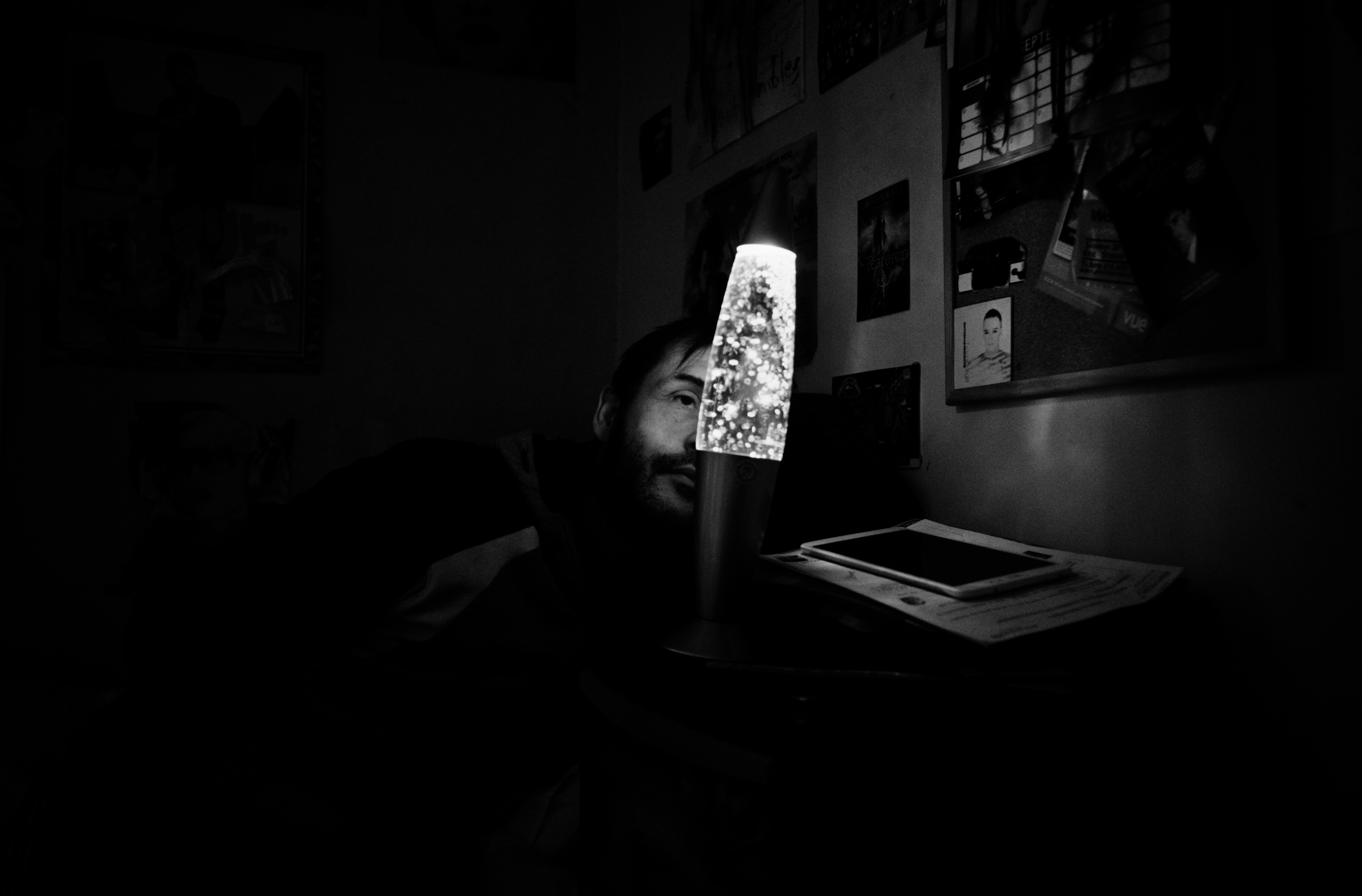
Lost in isolation.

Cut and paste collages, all have importance, all have meaning, nothing is without thought, nothing an aside.
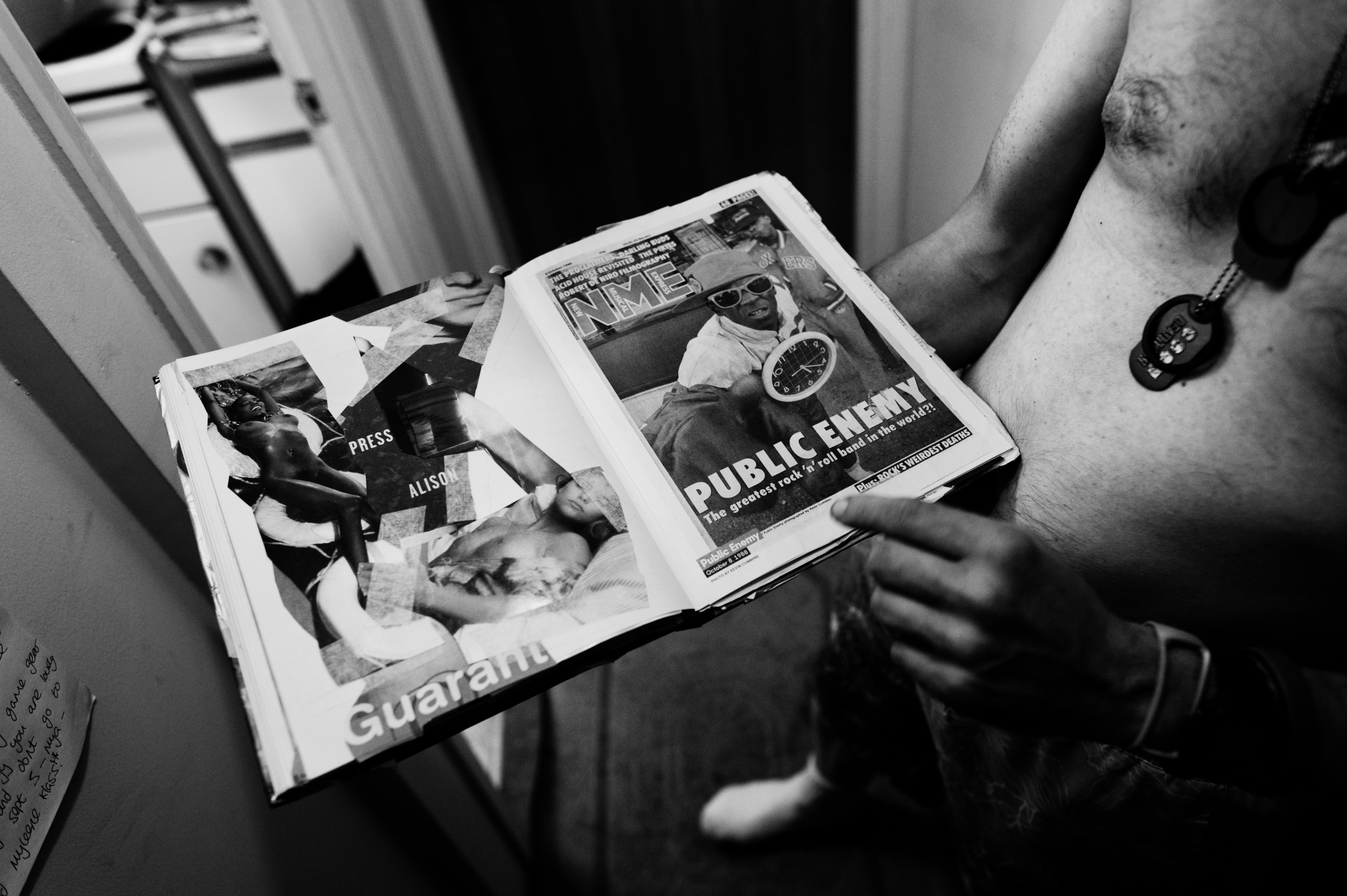
Explaining one of many collage journals, how words, images have their roots in memory and coincidence.
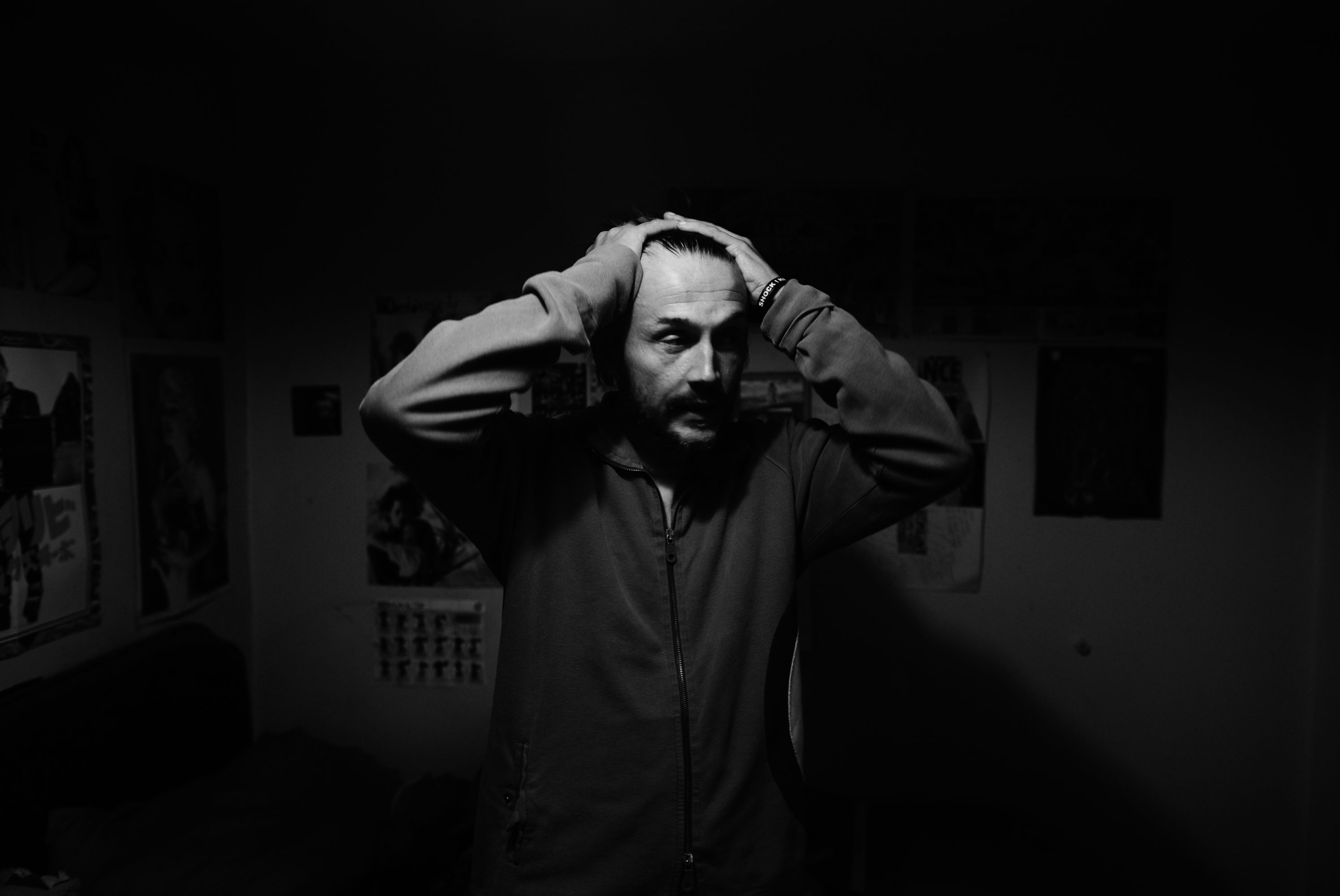
A moment of desperation, most always enhanced by the stress and pain of relentless loneliness.

Bags of medication, unopened for weeks, in Tilney1’s bathroom.

In a bid to quit his obsessive smoking habit, Tilney1 plastered his legs with anti-smoking patches.

After voluntarily visiting his local GP, suffering the crippling symptoms of his schizophrenia, their volume elevated after missing his medication for weeks and after little to no regular visits to ensure his well-being, a crisis team had been called and are inbound to admit Tilney1 to the psychiatric hospital.
Tilney1’s landline telephone had been cut off and he was only making calls to the mental health helpline provided by Mind, calls and contact he desperately needed but was trying to regulate as they were costing him a fortune on his mobile telephone. The stress of spiralling ever deeper in debt was becoming impossible to live with.

Always aware of his manic episodes, kidnapped, a passenger, under their power, exhausted from months of sleepless nights and days of isolation, Tilney1 is consumed with the fear and despair at imminently being hospitalised.

Awaiting the crisis team that will transport him to the psychiatric hospital, Tilney1 shares some of his self-portrait photography.

Slipping in and out of lucidity, Tilney1’s symptoms attain an ever more brutal grip.

A final cigarette before the crisis team arrives.

Shaved. Minutes later, the crisis team arrived and Tilney1 was taken to the acute admission ward within Hellesdon psychiatric hospital in Norwich (NSFT) for a month.
A record number of patients are dying unexpectedly each month at Norfolk and Suffolk’s troubled mental health trust, despite years of reassurances and reviews into the problem. Eighty-seven men and women who had been cared for by the Norfolk and Suffolk Foundation Trust (NSFT) died unexpectedly from January to May, 2016.
In April and May 2016, twenty-one people died.
An unexpected death is classified as a death where the cause could not be anticipated. It could be natural causes, suicide, a physical illness or an accident and includes anyone who has been treated by the trust in the six months before their death.
I spoke with Terry Skyrme, a retired social worker and Approved Mental Health Professional (AMHP) who devotes and dedicates his time in retirement to campaigning to save mental health services.
“I was working in mental health in London and we moved to Norfolk and I got a job in Norfolk in 1996 with what was called the ‘Assertive Outreach Team’, which was an absolutely fantastic team.”
“It had two psychiatrists, two psychologists, support workers, three social workers, it was what you’d call a genuinely multi-disciplinary team. During the early 1990’s there had been a whole number of tragedies, the Christopher Clunis murder, Ben Silcock jumping into the zoo in London.”
“These AOT’s were the kind of teams set up in the wake of these tragedies in the early 90’s and the team we had set up in Norfolk was the real model, the full model. Then over time, I date it back to when it became a foundation trust, they started running it down.”
“The government imposed cuts across the board on the NHS, 20 billion pounds of ‘efficiency savings’ cuts and cost saving and in Norfolk and Suffolk that translated into 40 million pounds of cost saving over three years.”
“What the local Norfolk Trust decided to do, to make these savings was to impose a radical redesign, an incredible cutting of both the in-patient and out-patient service but there was no way to cut it, it was already an underfunded service. Instead of two psychiatrists, one psychiatrist, gradually social workers were reduced, it was run down and by 2012 -13 there were two of these specialist teams, one covering Norwich and one covering the county and when they announced the 40 million pounds worth of cuts over a three year period, they abolished both of those teams overnight.”
“AOT teams were set up to catch people who are so unwell that they can’t engage with the average community mental health team, the AOT’s were designed so they could engage with people who were hard to engage with, people who wouldn’t necessarily keep appointments or keep taking their medication, kept relapsing, were in and out of hospital.”
“They abolished two assertive outreach teams and the three community mental health teams that covered the whole of central Norfolk, they were reduced down to two teams. The AOT’s were really well staffed, they had to be. For example, you’d go out in the morning and if somebody wasn’t in or didn’t answer the door you could go back later in the day. The outreach community health nurse couldn’t do that, so they were specialist teams targeting the most severely mentally ill.”
“AOT’s were based on research, based on a model in Australia whereby, basically, instead of offering just a medical model to somebody, they would offer almost like a bargain, you would say to the person “What do you want to achieve?, what do you really need help with?” and in return, that’s how the engagement would be made. In return, you would get to know the person, you might be able to help them develop some insight into their illness, that’s how the teams worked and they worked in a holistic way not a purely medical way, these were the teams that were axed overnight, both abolished in 2013 and their caseloads were just absorbed into the general community mental health teams, who themselves were cut by a third.”
“More or less every GP surgery had a CPN (Community Psychiatric Nurse) attached to them, for example, if somebody came into to see their GP they could be told “If you come in next week, you can see the CPN” and the CPN could then decide does that person need specialist mental health services or could they be helped by a few sessions with themselves or could they advise the GP. These CPNs were called link workers, qualified nurses linked to GP surgeries, following the cuts, they all went in the radical redesign. All the band six staff (Fully qualified CPN) were cut and so then were forced to apply into competition with one another for their own jobs. People working here were obviously getting stressed out of their heads what with the link workers being abolished the community mental health teams cut. So, the crisis team found themselves absolutely chock a block with cases, completely full up. The staff are very caring but they’re struggling to do a good job because they’re so stretched.”
“Crisis teams would often work with people for a month, two months, three months until the crisis was over and then transfer them back to the community mental health team, what we found was that the community mental health teams were full up, they had hundreds of allocated cases, every aspect of the service was cut, including in-patient beds.”
“We reached a peak in 2014 where 40 patients from our area ended up placed in private hospitals all across the country. What this meant for us as AMHPs is that we could no longer practise safely, professionally, ethically, and sometimes, it felt, not lawfully. Informal admissions (as opposed to compulsory admissions under the Mental Health Act) became more difficult to arrange; the safe, human conveyance (transport) of patients became more difficult to ensure, and alternatives to hospital admission ceased to exist.”
“Locally we saw a rise in unexpected deaths of patients under our so-called care. As AMHPs we called for meetings with the chief executive, we wrote to the CQC, to Norman Lamb, our local NHS commissioners and others but to little substantial effect. Our own trust continued to deny a crisis and even claimed they were enhancing community services.”
“Since November 2013, I have been part of a group that launched a Campaign to Save Mental Health Services in Norfolk and Suffolk. We have been successful in uniting staff, patients, relatives, trade unions and community groups under our banner.”
Released from Hellesdon hospital, Tilney1 explains some of the artworks that he produced during his stay.
“Sometimes making work in the hospital can be really heavy but at the bottom of this piece, I wrote lots of nice things, like how worried I was for all the other people in the hospital with me whilst I was there.”

First night home after being released, Tilney1, was completely terrified, disoriented and within an evident state of shock. During his stay in the hospital, his medication had been altered and he was yet to fully adjust to their effects.
“The doctors and nurses, they all say I’m not a psychopath, I’m not this, I’m not that and they are nice, all the time and the people that work in mental health, they must come under extreme stress and themselves go off ill, due to being so stressed.”
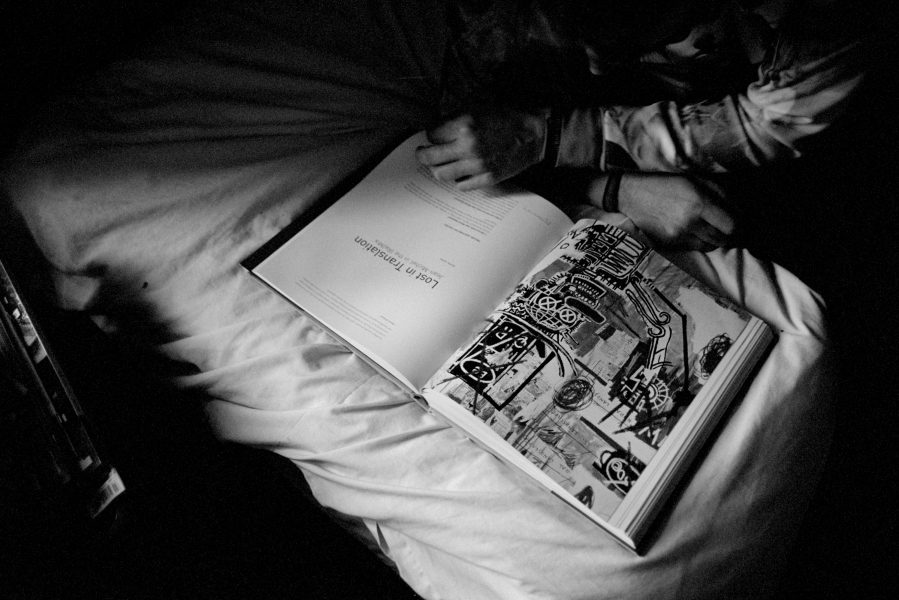
Back at home, Tilney1 attempts to adjust to the new medication and to fill the loneliness with studies.

With the new medication now noticeably working, whilst being monitored by visiting nurses, Tilney1 returns to making photographs.

“When you see a news report about someone beating someone up in a hospital because they weren’t getting the right medication or doing something bad because they weren’t getting the correct help, you see a picture of him. When you see negative things about people with mental illness, you feel that’s how people feel about you.”
“I have this incredible insight, about my illness, sometimes I think, like the doctors who come to see me. I said I wanted to go to church and a support worker asked me “You want to go and repent?” so I looked up what repent meant on Google but I’m not going to church to repent, I’m just going because I am a nice person and it interests me, why would they even mention repenting?. That’s the thing you see, it’s just low intellect, what they say, in an enlightened world, you should be able to like the band Nirvana and go to church.”
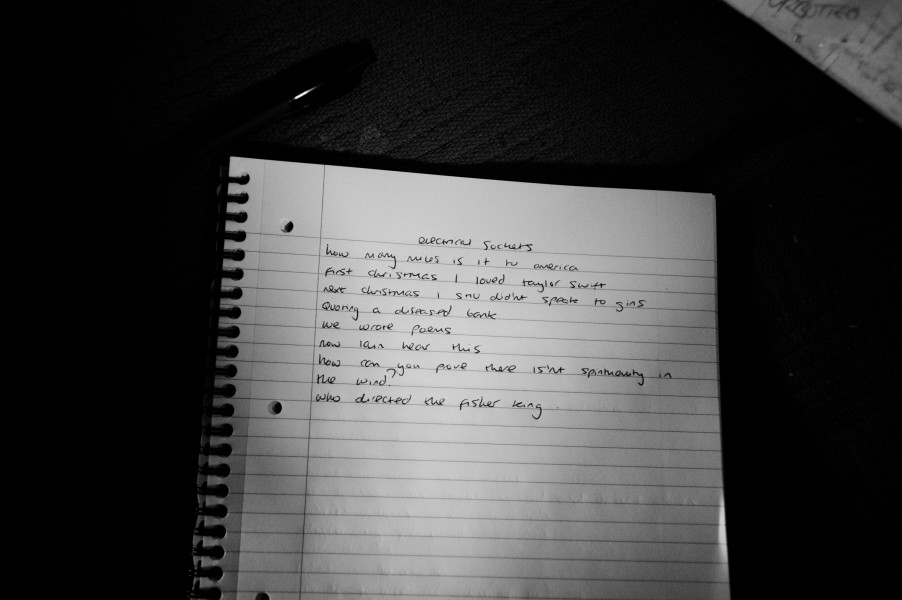
Writing poems.

“I really wish that when all my spending went out of control, I mean, I can’t go back in time and change it, if I could come off cigarettes and enjoy life but I can’t change anything once it’s happened.”
“Keeping a dream diary, recalling everything has turned me into a poet.”

Tilney1’s cassette recorder, used to document thoughts and record spoken word poetry.

“Basically, after my original CPN (Community Psychiatric Nurse) left, in my loneliness, things started to go wrong.”
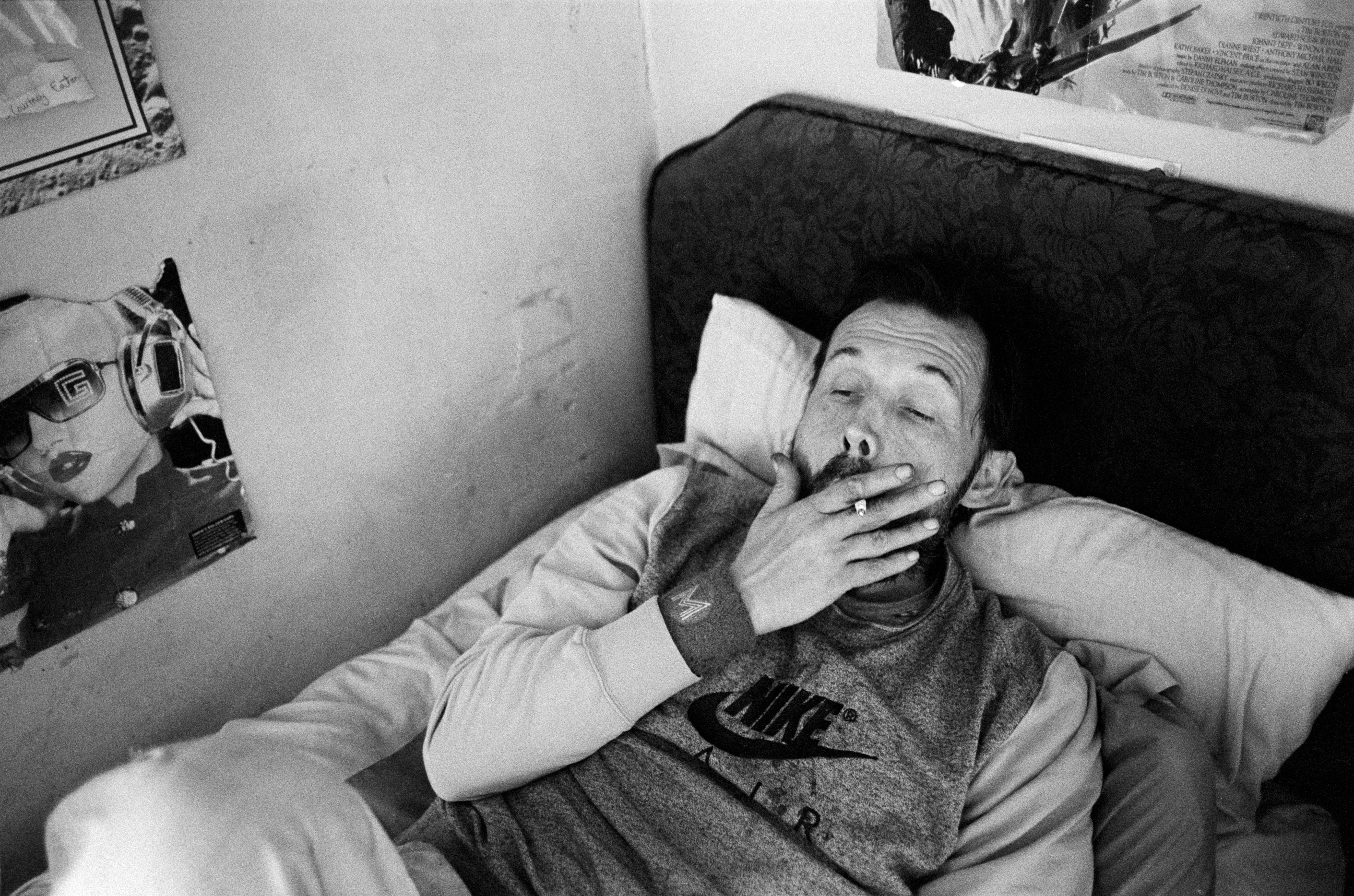
With a tapering off of the support to ensure Tilney1 regularly sticks to his medication, his symptoms began to take control again.
“I’d left the door (Of my apartment) open so the mental health crisis team could get in, I took my medication in the morning, instead of the evening before, I fell asleep, hoping that they would be able to get in (The door to Tilney1’s apartment block has a security door and buzzer system) and come in and see me, but they couldn’t get in.”

Tilney1’s cassette recorder.

Making a final recording before the crisis team arrive to take Tilney1 to psychiatric hospital, for the second time in three months. However, due to a lack of available bed’s at Norwich’s acute admission ward within Hellesdon Hospital (Norfolk and Suffolk NHS foundation trust) Tilney1 is to be placed in Mundesley private mental health facility, a sixty mile round trip away from home.

“I took my medication last night and I’m trying not to dwell on the first thought that enters my head. All my thoughts are just… and the constant smoking… I just don’t know what to do anymore. The crisis team is coming to see me soon to take me to hospital.”

11 Comments
Mike Hartley
August 2, 2016 at 9:32 amTilney1, Jim … thank you for sharing this story. Tilney1 … I hope you find some stability and are able to keep trying, you are so strong. This world is not fair. Your story reminds us of how mindful we need to be.
JA Mortram
August 2, 2016 at 8:07 pmThank you!. X
Javi
August 28, 2016 at 4:16 pmThanks for sharing this great story. My best to Tilney1. Keep up the good work. X.
Hannah May
November 7, 2016 at 12:55 amIncredible story and incredible work, thank you for sharing.
I hope all the best for Tilney1, your work and his corporation to document is inspiring !
Thanks again.
Zelda Cheatle
January 27, 2017 at 11:34 amWhat a powerful story and great pictues, really showing Tilney1 from the inside out. I am really moved – by the lonlieness, having to cope with such an engulfing illness all by yourself, how terrifying life can be when you are ill. I am so glad this collaboration happened between you. The power of pictures.
JA Mortram
January 30, 2017 at 6:47 pmThank you!.
lisa
May 22, 2017 at 12:15 pmHow desperately sad that people who are well-known to mental health services are just abandoned and left to drift back in to crisis before they can access any kind of support. Inhumane and cruel, and so many people have relapsed after a care co-ordinator they had a good relationship was forcibly removed either because of “reorganisation” or they were made redundant. The local mental health trust printed lots of booklets of their “vision and values” – one of which is “no decision about me, without me”. Yet one of the most fundamental aspects of the care and support someone receives is the named worker that they have, who they trust to build up a relationship with, who they tell their inner most troubling thoughts to… managers so far removed from face to face client care move workers around like chess pieces on a board, seemingly oblivious or uncaring to the impact on the person they were working with. it’s so sad also that people in need of support themselves are worried about the mental well-being of the staff trying to support them. We should be able to be confident, strong, optimistic and holding on to hope in our supportive relationships, but as we push ourselves on day-to-day it seeps through and we know we are fooling no one, and that those we are meant to care for see it. We are letting people down, because we too are being let down.
JA Mortram
June 11, 2017 at 3:57 pmLisa, thank you so much for your comment and your insight. I agree, at the moment, everyone is being let down and it’s utterly, utterly unforgivable and heartbreaking.
Steve Sloan
August 27, 2020 at 1:46 pmThe story of TiIney1 is an allegory of our times . This is extraordinary work of huge importance and quality and speaks of the value that we fail to assign to people as individuals.
Left wondering to know more, sense of voyeurism in wanting to know that but a sense of relief too that I do want to know.
My best wishes to Tilney1
Colin cleave
June 19, 2022 at 1:58 amJim …beautiful photos, moving story.
Just discovered your work, your an artist.
Regards from
New Zealand
Mark Osborn
October 18, 2022 at 12:02 pmJim,
Found your work via Sean Tucker. Just have to say how important these images are, along with the stories they tell. It’s heartbreaking that these lived experiences go on all around us, without wider visibility. It really makes you stop and think about how we (society) prioritise our resources,
Best wishes,
Mark Osborn